




 he physiological risks of magnetic and radiofrequency fields have been intensively examined for a long time. There is, for instance, danger of radiofrequency heating, of shear forces between brain tissues, nerve stimulation by gradient fields, as well as genotoxic effects. There are reports about sensations of vertigo, nausea, and metallic taste at 3 and 7 Tesla.
he physiological risks of magnetic and radiofrequency fields have been intensively examined for a long time. There is, for instance, danger of radiofrequency heating, of shear forces between brain tissues, nerve stimulation by gradient fields, as well as genotoxic effects. There are reports about sensations of vertigo, nausea, and metallic taste at 3 and 7 Tesla.
Yet, there are hardly any long-term studies following persons who were exposed to such fields. To get an impression of the complexity of the topic we shall discuss some possible physiological hazards in more detail on the following pages. A number of topics require further evaluation, in particular concerning ultrahigh magnetic fields.
In every MR examination, a large static magnetic field is applied. Field strengths for clinical equipment can vary between 0.2 and 3.0 T (even 7 Tesla in some regions); to date, experimental imaging units have a field strength of up to 17.5 T (Table 18-01).
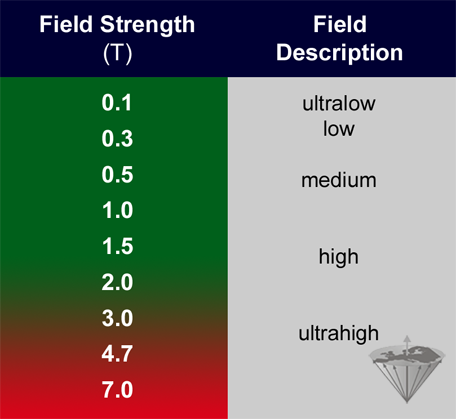
Table 18-01:
Definition of field strength. Ultralow-field machines operate at a field strength below 0.1 T, low field between 0.1 and 0.5 T, medium field between 0.5 and 1 T, high field between 1 and 2 T, and ultrahigh field machines above 2 T (Definitions set by EMRF in 1989).
There are a number of biophysical effects whereby static magnetic fields might influence biological processes or an organism's behavior. Hoff and collaborators stress that forces on metallic implants and radiofrequency power deposition and heating are safety considerations at 7 T. Patient bioeffects such as vertigo, dizziness, false feelings of motion, nausea, nystagmus, magnetophosphenes, and electrogustatory effects are more common and potentially more pronounced at 7 T than at lower field strengths [⇒ Hoff 2019].
 Vestibular system. In 1988 a group at the General Electric Corporate Research and Development Center described in an abstract sensations of vertigo, nausea, and metallic taste in a group of volunteers. There was statistically significant evidence for field-dependent effects which were greater at 4 T than at 1.5 T. In addition, they found magnetic phosphenes caused by motion of the eyes within the static field. The results were published in a full paper in 1992 and considered proof that there is a sufficiently wide margin of safety for the exposure of patients to the static fields of conventional magnetic resonance equipment operated at 1.5 to 2 T and below [⇒ Schenck 1992].
Vestibular system. In 1988 a group at the General Electric Corporate Research and Development Center described in an abstract sensations of vertigo, nausea, and metallic taste in a group of volunteers. There was statistically significant evidence for field-dependent effects which were greater at 4 T than at 1.5 T. In addition, they found magnetic phosphenes caused by motion of the eyes within the static field. The results were published in a full paper in 1992 and considered proof that there is a sufficiently wide margin of safety for the exposure of patients to the static fields of conventional magnetic resonance equipment operated at 1.5 to 2 T and below [⇒ Schenck 1992].
More than twenty years later, scientific articles and two PhD theses from the Netherlands threw new light on hazards of ultrahigh field magnetic resonance equipment operating at fields higher than 2 Tesla, describing reversible decline in cognitive function as well as symptoms of nystagmus, vertigo, postural instability, nausea, and metallic taste in employees working with MRI at fields of 3 T and, to a higher degree, at 7 T [⇒ Roberts 2011, ⇒ Schaap 2015, ⇒ van Nierop 2015].
One third of the severely ill patients enrolled in a comparative study at 7 Tesla complained about vertigo and nausea caused by the equipment [⇒ Springer 2016].
These symptoms, with the exception of the observed change of taste, hint to an effect of the magnetic field on the vestibular system that is responsible for the sense of balance, spatial orientation, and posture which was substantiated by Houpt and colleagues. They observed that rats did not enter a 14.1 T magnet. After a first climb into 14.1 T, most rats refused to re-enter the magnet or climb past the 2 T field line. Detection and avoidance required the vestibular apparatus of the inner ear, because after surgical removal of the labyrinth rats readily traversed the magnet [⇒ Houpt 2007].
It is not advisable to prescribe histamine-blockers such as diphenhydramine to preventively mitigate the strength of vertigo and nausea at ultrahigh static magnetic fields, although this procedure has been proposed to "pave the way to even higher field strength" [⇒ Thormann 2013].
Such patients should rather be referred to lower field machines.
Some additional results are contradictory and cannot be explained by biophysical or biochemical mechanisms. The effects observed may be attributed to other causes not considered by the researchers in the setup of the experimental protocol.
 Volume forces — shear forces. Volume forces are dependent on tissue susceptibility and the product of field strength and spatial field gradient. Their threshold for human tolerance is still unknown.
Volume forces — shear forces. Volume forces are dependent on tissue susceptibility and the product of field strength and spatial field gradient. Their threshold for human tolerance is still unknown.
There is also limited knowledge about the susceptibility differences between iron containing tissues in the cerebral cortex and surrounding tissues and possible shearing issues at ultrahigh magnetic fields, such as subtle variations in the magnetic properties of brain tissue, possibly reflecting varying iron and myelin content [⇒ Fukunaga 2010].
 Nerve conductivity. As early as 1893, the first results of experiments about a possible influence of static magnetic fields upon nerve tissue were obtained [⇒ D’Arsonval 1893]. These and all later experiments showed negative results. There are apparently no effects on the conduction of impulses in the nerve fiber up to a field strength of 0.1 T generated by either changing the electrical resistance or the potential of the excitation [⇒ Abashin 1975, ⇒ ACR 2007].
Nerve conductivity. As early as 1893, the first results of experiments about a possible influence of static magnetic fields upon nerve tissue were obtained [⇒ D’Arsonval 1893]. These and all later experiments showed negative results. There are apparently no effects on the conduction of impulses in the nerve fiber up to a field strength of 0.1 T generated by either changing the electrical resistance or the potential of the excitation [⇒ Abashin 1975, ⇒ ACR 2007].
The minimum magnetic field required to produce observable effects seems to be quite large. Theoretical considerations argue that fields of 24 T are required to produce a 10% reduction of nerve impulse conduction velocity [⇒ Wikswo 1980].
 Changes in enzyme kinetics. Up to 45 Tesla, no important effects on enzyme systems have been observed.
Changes in enzyme kinetics. Up to 45 Tesla, no important effects on enzyme systems have been observed.
 Orientation changes of macromolecules, living cell subcellular components, and magneto-biomaterials in the brain. A re-orientation caused by diamagnetic anisotropy is seen in highly ordered biological structures, such as sickle cells and retinal rods in magnetic fields of 0.35 and 1.0 Tesla, respectively. While it is not possible to orient the individual constituent molecules with such fields, these structures can be oriented as a whole by summing the anisotropy over a large number of mutually oriented molecules. These results are reproducible [⇒ Hong 1995].
Orientation changes of macromolecules, living cell subcellular components, and magneto-biomaterials in the brain. A re-orientation caused by diamagnetic anisotropy is seen in highly ordered biological structures, such as sickle cells and retinal rods in magnetic fields of 0.35 and 1.0 Tesla, respectively. While it is not possible to orient the individual constituent molecules with such fields, these structures can be oriented as a whole by summing the anisotropy over a large number of mutually oriented molecules. These results are reproducible [⇒ Hong 1995].
It is still unknown what happens to magneto-biomaterials in the human brain at high and ultrahigh fields; it is also still unknown what their function is — whether they are for instance bioreceptors or biosensors [⇒ Kirschvink 1992, ⇒ Schultheiss-Grassi 1999].
Biogenic magnetite in the human brain was detected as a minimum of 5 million single-domain crystals per gram for most tissues in the brain and greater than 100 million crystals per gram for pia and dura. Magnetic property data indicate the crystals are in clumps of between 50 and 100 particles. Apparently, such nanoparticles can also be incorporated into the brain by breathing in polluted air.
 Magnetohydrodynamic effects. In a model of the human vasculature it was shown that changes in hydrostatic pressure in the presence of a large static magnetic field (10 Tesla) were less than 0.2% [⇒ Keltner 1990].
Magnetohydrodynamic effects. In a model of the human vasculature it was shown that changes in hydrostatic pressure in the presence of a large static magnetic field (10 Tesla) were less than 0.2% [⇒ Keltner 1990].
These changes are claimed to be caused by interaction of induced electrical potentials and currents within a solution, e.g. blood, and an electrical volume force causing a retardation in the direction opposite to the fluid flow. This decrease in flow velocity must be compensated for by an elevation in pressure. At and below 1.5 T no significant changes are expected [⇒ Budinger 1986, ⇒ Tenforde 1983].
 Membrane transportation and blood sedimentation. Other potential hazards from static fields include, for instance, membrane transportation and blood sedimentation induced by the field. As Mansfield pointed out, static magnetic field gradients of 0.01 T/cm make no significant difference in the membrane transport processes. The influence of a static magnetic field upon erythrocytes is not sufficient to provoke sedimentation, as long as there is a normal blood circulation [⇒ Mansfield 1981].
Membrane transportation and blood sedimentation. Other potential hazards from static fields include, for instance, membrane transportation and blood sedimentation induced by the field. As Mansfield pointed out, static magnetic field gradients of 0.01 T/cm make no significant difference in the membrane transport processes. The influence of a static magnetic field upon erythrocytes is not sufficient to provoke sedimentation, as long as there is a normal blood circulation [⇒ Mansfield 1981].
 Cardiac changes. A field-strength-dependent increase in the amplitude of the ECG in rats has been observed during exposure to homogeneous stationary magnetic fields. The minimum level at which augmentation could be observed was 0.3 T; at 2.0 T, the increase was by an average of 400%. The augmentation in T-wave amplitude occurred instantaneously and was immediately reversible after exposure to the magnetic field ceased (Figure 18-10). There have been no abnormalities in the ECG in later follow-up. The authors suggest that augmentation of the signal amplitude in the T-wave segment may result from a superimposed electrical potential [⇒ Gaffey 1981].
Cardiac changes. A field-strength-dependent increase in the amplitude of the ECG in rats has been observed during exposure to homogeneous stationary magnetic fields. The minimum level at which augmentation could be observed was 0.3 T; at 2.0 T, the increase was by an average of 400%. The augmentation in T-wave amplitude occurred instantaneously and was immediately reversible after exposure to the magnetic field ceased (Figure 18-10). There have been no abnormalities in the ECG in later follow-up. The authors suggest that augmentation of the signal amplitude in the T-wave segment may result from a superimposed electrical potential [⇒ Gaffey 1981].
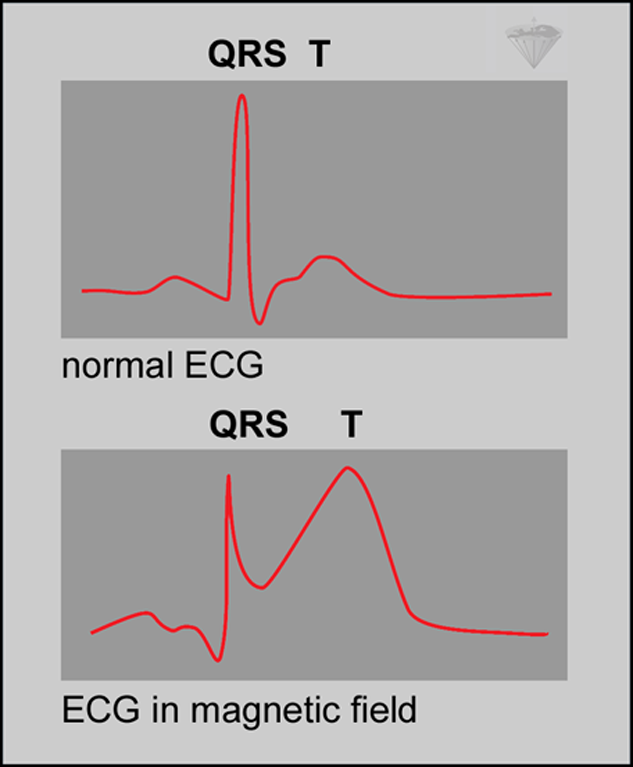
Figure 18-10:
Flowing blood can behave as a moving conductor in a magnetic field. The field can induce a voltage that will be highest during the part of the cardiac cycle with the fastest blood velocity. This coincides with the T-wave of the ECG and enhances the T-wave, potentially mimicking pathology.
At field strengths of between 7 and 10 T, no arrhythmia could be proven [⇒ Battocletti 1981]. According to the national radiation protection agencies, it is unlikely that cardiac fibrillation occurs as a result of induced flow potential in the major blood vessels or heart chambers at this level of field intensity.
No circulatory alterations coincide with the ECG changes. No biological risks are believed to be associated with them.
 Genetic effects. There have been several reports that static magnetic fields may provoke genetic mutations, changes in growth rate and leukocyte count and other effects; however, some results of these experiments could be reproduced, others could not [⇒ Schwartz 1982, ⇒ Vijayalaxmi 2015].
Genetic effects. There have been several reports that static magnetic fields may provoke genetic mutations, changes in growth rate and leukocyte count and other effects; however, some results of these experiments could be reproduced, others could not [⇒ Schwartz 1982, ⇒ Vijayalaxmi 2015].
Nevertheless, some authors claim it be unlikely that mutagenic effects are introduced by fields lower than 1.0 T [⇒ Mansfield 1981], in additoon, there is no convincing evidence for a genotoxic effect from MRI up to 7 T [⇒ Budinger 2016], although, for instance, Takashima and collaborators described genotoxic effects in DNA-repair defective mutants of drosophila melanogaster after 24-hour exposure to static magnetic fields of 2, 5, and 14 T [⇒ Takashima 2004].
Varying magnetic fields are necessary for the localization of nuclei with magnetic properties within the sample.
 Magnetic phosphenes are a well described effect of varying magnetic fields. They were first observed in the late 19th century [⇒ D’Arsonval 1896].
Magnetic phosphenes are a well described effect of varying magnetic fields. They were first observed in the late 19th century [⇒ D’Arsonval 1896].
Phosphenes are stimulations of the optic nerve or the retina, producing a flashing sensation in the eyes. They seem not to cause any damage in the eye or the nerve. They are attributed to magnetic-field variations, but difficult to create in common clinical systems and may start occurring in a threshold field change of between 2 and 5 T/s. Motion-induced magnetic phosphenes were easily visible at 4 Tesla [⇒ Schenck 1992].
 Electrogustatory effects are claimed not to be connected to the presence of metallic tooth-fillings. An exact threshold could not be determined. It seems to be set off by the motion of the head, depending on rate and direction.
Electrogustatory effects are claimed not to be connected to the presence of metallic tooth-fillings. An exact threshold could not be determined. It seems to be set off by the motion of the head, depending on rate and direction.
However, one experimental publication hints that in an ex vivo setting, mercury may be released from amalgam fillings after exposure to 7.0 Tesla but not at 1.5 Tesla [⇒ Yilmaz 2018].
 Peripheral nerve stimulation (PNS). The mean threshold levels for various stimulations are 3600 T/s for the heart, 900 T/s for the respiratory system, and 60 T/s for the peripheral nerves. They increase with field [⇒ Budinger 1991].
Peripheral nerve stimulation (PNS). The mean threshold levels for various stimulations are 3600 T/s for the heart, 900 T/s for the respiratory system, and 60 T/s for the peripheral nerves. They increase with field [⇒ Budinger 1991].
Guidelines in the United States limit switching rates at a factor of three below the mean threshold for peripheral nerve stimulation.
Varying magnetic fields are also used to stimulate bone healing in non-unions and pseudarthroses. The reasons why pulsed magnetic fields support bone healing are not completely understood [⇒ Bassett 1982].
Rapid echo-planar imaging and high-performance gradient systems create fast-switching magnetic fields inducing currents that stimulate muscle and nerve tissues (cf. EPI).
Radiofrequency pulses are used in MR imaging for the excitation of the nuclei.
 Extremely low-frequency (ELF) fields. Their influence has been blamed for numerous reactions, occurrences and diseases in animals and humans, for instance cancers, Alzheimer's disease, or even causing a decrease in milk production in cows.
Extremely low-frequency (ELF) fields. Their influence has been blamed for numerous reactions, occurrences and diseases in animals and humans, for instance cancers, Alzheimer's disease, or even causing a decrease in milk production in cows.
The most likely best known publications among articles about this topic are those associating an increase in the incidence of leukemia with the location of buildings close to high-current power lines with ELF electromagnetic radiation of 50-60 Hz, and industrial exposure to electric and magnetic fields. In 1979, Wertheimer and Leeper reported an association between childhood cancer and electrical current configuration of houses in Denver, Colorado [⇒ Wertheimer 1979]. This publication provoked a torrent of questions and research programs [⇒ Milham 1982, ⇒ Willett 2003].
To date, there is neither a final confirmation of a connection nor is there a corroboration of the contrary. Anyway, a transposition of such effects to MRI seems rather unlikely, if they exist at all.
Because of the nearly unlimited number of variables it is nearly impossible to collect unbiased statistics in huge populations; for instance, the death toll caused by air pollution is orders of magnitude higher than the claimed toll by leukemia caused by ELF.
 Heat deposition. RF fields may interact with both tissues and foreign bodies, such as metallic implants, in the patient. The main result of this type of interaction is heat.
Heat deposition. RF fields may interact with both tissues and foreign bodies, such as metallic implants, in the patient. The main result of this type of interaction is heat.
The higher the frequency (and thus magnetic field), the larger will be the amount of heat developed; and the more ionic the biochemical environment in the tissue, the more energy that will be deposited as heat [⇒ Led 1978, ⇒ NRPB 1981, 1992].
This effect is well-known for homogeneous model systems, but the complex structure of various human tissues makes detailed theoretical calculations very difficult, if not impossible.
RF power deposition and thus heating are increased by changing MR parameters such as decreasing the RF repetition time, adjusting flip angles, and changing matrix size [⇒ Bottomley 1981, ⇒ Mollerus 2010].
In several in vitro and in vivo low and medium field experiments, no life threatening increase in temperature could be shown. Even in high magnetic fields, no local temperature increase greater than 1° C occurred [⇒ Budinger 1986, ⇒ Liboff 1965].
The highest skin temperature increase described in humans reached 2.1° C [⇒ Shellock 1994], however in the uterus of pregnant animals at ultrahigh field (3 Tesla) 2.5° C were measured [⇒ Cannie 2016].
 Eddy currents may heat up implants and thus may cause local heating. In vitro worst-case experiments performed with a large and very thin thermally insulated aluminum sheet at 1.5 T after 15 minutes of exposure showed a temperature rise of only 0.08°C.
Eddy currents may heat up implants and thus may cause local heating. In vitro worst-case experiments performed with a large and very thin thermally insulated aluminum sheet at 1.5 T after 15 minutes of exposure showed a temperature rise of only 0.08°C.
 Hot spots may occur in the exposed tissue. At present, it seems unlikely that such hot spots in the body exist, but to avoid or at least minimize effects of such theoretical complications, the frequency and the power of the RF irradiation should be kept at the lowest possible level.
Hot spots may occur in the exposed tissue. At present, it seems unlikely that such hot spots in the body exist, but to avoid or at least minimize effects of such theoretical complications, the frequency and the power of the RF irradiation should be kept at the lowest possible level.
 The Specific Absorption Rate (SAR) helps to estimate RF heating effects. It might be a poor indicator of magnetic resonance-related implant heating [⇒ Nitz 2005]. However, SAR is regulated and MR operators are required to follow these regulations.
The Specific Absorption Rate (SAR) helps to estimate RF heating effects. It might be a poor indicator of magnetic resonance-related implant heating [⇒ Nitz 2005]. However, SAR is regulated and MR operators are required to follow these regulations.
SAR increases with field strength, radiofrequency power and duty cycle, as well as transmitter coil type and body size. In high and ultrahigh fields, some pulse sequences or procedures may create a higher SAR than recommended by the agencies.
At low fields, the maximum SAR is at the surface; this changes if the field strength is increased to high and ultrahigh fields. With the exception of the eyes, the human head, for instance, has good heat removal mechanisms for its surface, but not for the brain. As Hoult pointed out in a review paper [⇒ Hoult 2000], caution is called for when imaging at ultrahigh fields.