




![]() n the early 1980s, MR imaging started being clinically evaluated. One of the most admirable research groups worked at Hammersmith Hospital in London. The head of the group was Robert E. Steiner, but Ian R. Young and Graeme M. Bydder were the moving forces. Among others, Frank H. Doyle and Jacqueline M. Pennock supplemented this group.
n the early 1980s, MR imaging started being clinically evaluated. One of the most admirable research groups worked at Hammersmith Hospital in London. The head of the group was Robert E. Steiner, but Ian R. Young and Graeme M. Bydder were the moving forces. Among others, Frank H. Doyle and Jacqueline M. Pennock supplemented this group.
Because MR imaging is at the crossroads between medicine, biology, chemistry, physics, as well as data processing, research groups with strong interdisciplinary relationships and cross-fertilization became scientifically extremely fruitful, …
… which led to the 'odd couple' system, involving one physician and one scientist. At congresses, you would always see Ian Young together with Graeme Bydder (Figure 20-41), a seemingly ideal combination.
There were other couples like them (e.g., Rinck and Muller, Figure 20-42), but apparently such an interdisciplinary relationship between radiologists and physicists or chemists does not fit into all European academic systems.
Figure 20-41:
Graeme Bydder (left) and Ian Young (1932-2019).
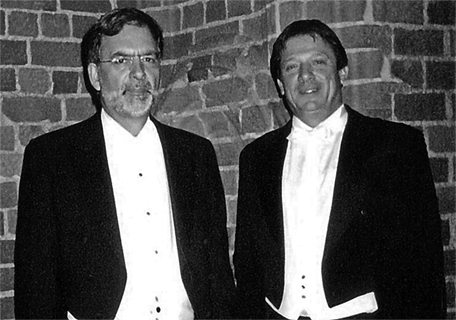
Figure 20-42:
Peter A. Rinck (left) and Robert N. Muller (at the 2003 Nobel Prize presentation to Paul C. Lauterbur and Peter Mansfield).
Early clinical imaging was extremely difficult, time-consuming, and often disappointing. Just chosen as an example: The first MR images were based upon proton-density differences, later upon differences in T1-weighting. Spin-echo imaging, for instance, was a bigger step than many would imagine. Today it is taken for granted and mostly replaced by faster echo techniques; but it has helped MR imaging immensely to become a routine technique.
By 1982-1983, the Hammersmith and Wiesbaden groups pointed out that long heavily T2-weighted multiecho SE sequences were better at highlighting pathology (Figure 20-43) [⇒ Bydder 1982; ⇒ Rinck 1983]. There were similar groups in Germany and in the United States, mostly in New England and California.
Figure 20-43:
Spin-echo images from 1984 of a recurrent brain tumor taken on a 0.14 Tesla system; TEs (a-d) between 20 and 300 ms.
Long echo times in multiecho CPMG sequences were a major leap forward in the first half of the 1980s. It took some years until T2-weighted images were generally accepted, mostly because many companies claimed that long TE was neither possible nor necessary.
The images were made five years before the introduction of Gd-based contrast agents; the tumor can be best delineated on image (d) at a TE of 300 ms.
Illustration from: Rinck PA, Bydder GM, and Harms SE. Magnetic resonance imaging of the brain. Published in the first edition of this textbook in 1985.
Unfortunately it is beyond the scope of this short introduction to mention all workers from around the world who can claim just credit for helping to advance the field — which is not meant to belittle their contributions to MR imaging. We mention first and foremost our own work, that of our collaborators, students and academic colleagues because we are most familiar with it — and can assess and judge it.
 In the 1980s and 1990s, magnetic resonance imaging was the latest diagnostic modality in medical imaging. It competed with other imaging methods and the questions were: "When do you use what?" and "What is and will be the impact of MR imaging upon the health system?"
In the 1980s and 1990s, magnetic resonance imaging was the latest diagnostic modality in medical imaging. It competed with other imaging methods and the questions were: "When do you use what?" and "What is and will be the impact of MR imaging upon the health system?"
Evaluation studies of the use of MR imaging had been already performed in the mid 1980s. However worthwhile these studies were, they came too early when the technology was still immature. Rapidly changing technology immediately invalidates such efficacy research. Some degree of technological stability is needed to encourage significant investment in it. For MRI, such an evaluation became possible after more than ten years of clinical use.
Thus, in October 1993, some thirty teams involving around 100 scientists met in Lugano, Switzerland, to try to reach at least a basic consensus. They had developed basic outlines of recommendations on how to apply MR imaging in certain diagnostic questions. This united effort was sponsored by two dozen international medical associations, a dozen commercial companies and World Health Organization. The main goal was to initiate the process of creating gamuts and diagnostic pathways for the proper application of MR imaging (Figures 20-44 and 20-45).

Figure 20-44:
Speakers at the opening session of the conference on "The Rational Use of Diagnostic Imaging" in Lugano, Switzerland, in 1993: Albert Baert (Antwerp), Josef Lissner (Munich), and Alexander Margulis (San Francisco) — introducing scientific MR imaging to a medical audience.
Figure 20-45:
Cover of the proceedings: "The Rational Use of Diagnostic Imaging".
The results were published in a 450-page book [⇒ Rational Use 1995]. In its foreword it is stated:
"During the three-year planning phase of this conference it became obvious that public agencies love statements about costs having to be cut, but other than making commonplace remarks they do not constructively contribute to cost-cutting efforts such as the one we try to perform here. For ministries of health all over Europe this effort is worthwhile, for the reimbursement and insurance agencies it is also worthwhile to reach a consensus; however, actually supporting such an endeavor does not seem to be part of their responsibilities. The task is then left to the rest of us and, so, the Lugano conference and this book represent our initial contribution …
"As is evident, the puzzle contains several pieces and perhaps has more than one solution. One indisputable feature was common to all participants in this meeting: the unequivocal belief in the benefits — present and potential — of MRI. The process of evaluation has begun and the road ahead will be determined by a conscientious action on the part of those involved. If the decisions on availability are not to be determined by cost alone and left in the hands of politicians and bureaucrats, the medical community and industry alike will have to continue this process of evaluation and achieve conclusive specifications on the clinical indications and future development of MRI."
A study published thirty years later found that 24% of MRI examinations were inappropriate and a comparison with a former study did not reveal an improvement but rather the opposite [⇒ Ståhlbrandt 2023].
About the only certainty in human affairs is that they are never in a steady state. The same holds for medical diagnostics and therapeutics in general. The pendulum of popular attitude is always swinging one way or the other and there is a permanent development which does not allow to reach a final conclusion. Perhaps a tighter supervision and more intensive interdisciplinary training might add to a more appropriate use of the technology.